Abstract
Introduction. Elderly patients (pts) with Immune thrombocytopenia (ITP) may represent a clinical challenge since comorbidities and impaired functional capacity may reduce the therapeutic landscape and drug tolerability.
Aims. To report ITP characteristics at diagnosis, and type/timing of treatment strategy, including response and toxicity rates in a cohort of elderly ITP pts.
Methods. An electronic database was established to retrospectively collect clinical/laboratory data on elderly (age ≥60 yrs) pts that received at least one line of therapy for ITP in 11 Italian Hematology Centers. Data cut-off was July 2018. Treatment decisions were at the physician's discretion. Diagnosis and responses were assessed according to current guidelines and terminology. Infectious, thrombotic and hemorrhagic complications were graded according to the WHO scale. Comparisons of quantitative variables between groups were carried out by Wilcoxon-Mann-Whitney rank-sum test, and association between categorical variables (2-way tables) was tested by χ2 test. Cumulative incidences of infections, bleeding, and thrombosis were calculated considering death as competing risk (Fine and Gray model). Statistical significance was set at p<0.05.
Results.Between January 1981 and January 2018, 526 ITP pts were diagnosed and treated in participating Centers. Median follow-up was 4.2 yrs (range: 0.25-24.4 yrs). Baseline characteristics of the total population were: median age 71.3 yrs (60-91.5); median platelet count 16 (1-99); number of pts with hemorrhages 134 (25.5%, grade 3-4: 6.3%).
All pts received a front-line therapy that was mainly based on prednisone (dexamethasone was used in 13.1% of the pts, regardless of age). Therapy was started at the time of diagnosis or in chronic phase in 75% and 16.9% of the cases, respectively; 94 pts (17.9%) had no response.
A second-line approach was required in 334 pts (63.5%) while 173 (32.9%) patients received also a third-line therapy; 76 (14.4%) pts required ≥4 treatment therapies. Eighty-four (16%) pts died; death was due to major hemorrhage in 9 pts, to thrombosis in 8 pts and to infection in 9 pts.
A total of 54 thromboses in 50 pts, 201 bleedings in 136 pts and 133 infections in 108 pts were observed during follow-up. Incidence rate of all-grade and ≥ grade-3 complications were: 4.60 and 1.15 per 100 pt-yrs (hemorrhages); 1.69 and 1.12 per 100 pt-yrs (thrombosis); 3.65 and 0.74 per 100 pt-yrs (infections).
Pts were sub-grouped into two categories according to age (elderly: 60-74 yrs, n.315, 59.9%; very elderly: ≥75 yrs, n.211, 40.1%). At diagnosis, bone marrow biopsy was performed more frequently in pts <75 yrs (68.5% vs 56.8% in the very elderly, p=0.007). Compared to elderly pts, very elderly had similar platelet count at diagnosis but presented more frequently with cardiovascular risk factors (83.4% vs 63.8%, p<0.001) and were more frequently treated with anticoagulants (15.6% vs 4.1%, p<0.001), resulting in a higher rate of bleedings at diagnosis (32.2% vs 21.3%, p=0.005).
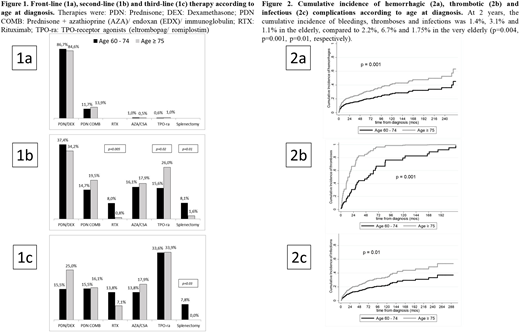
The type of front-line treatment was comparable across age groups (Figure 1A). Intensity (duration and dose) of prednisone treatment was not influenced by age, resulting in comparable response rates (16.5% and 14.7% of no-responders in elderly/very elderly pts, respectively; p=0.18).
Second-line, rituximab and splenectomy were most frequently used in pts aged <75, while very elderly received more frequently thrombopoietin-receptor agonists (TPO-ra) (Figure 1B). Third-line, splenectomy was reserved to patients aged <75, while the use of medical therapy was comparable across age groups (Figure 1C). After adjustment for the risk of death, the cumulative incidence of bleedings, thromboses and infections was significantly higher in the very elderly (p=0.004, p=0.001 and p=0.01) (Figure 2).
Conclusions. Very elderly pts were characterized by a higher frequency and severity of comorbidities and a higher need of chronic anticoagulant therapy, resulting in a more aggressive disease presentation. While first-line corticosteroid therapy was not influenced by age, very elderly pts were excluded from the use of splenectomy and exposed to an earlier use of TPO-ra. Overall, older age identified a more fragile population with a more severe disease course, in terms of hemorrhagic, thrombotic and infectious complications. Age-adapted treatment strategies should be further explored in elderly ITP pts.
Palandri:Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Cavo:AbbVie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; GlaxoSmithKline: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Adaptive Biotechnologies: Honoraria, Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees. Mazzucconi:Baxalta-Shire: Consultancy, Speakers Bureau; Bayer: Consultancy, Speakers Bureau; Novartis,: Consultancy, Speakers Bureau; Amgen: Consultancy, Speakers Bureau; Novo Nordisk: Consultancy, Speakers Bureau; CSL Behring: Consultancy, Speakers Bureau. Rodeghiero:Amgen, Novartis, Argenx: Consultancy, Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal